Hi everyone
We hope each of you had a lovely Festive Season, and the coming New Year is a healthy, happy and safe one for you and for your family.
With 22 January fast approaching, we want to remind you tickets are selling fast to the CRBF T20 Birthday Bash, with gates opening at 2 pm. The tickets have remained at $20 per person which includes barbecue and entry. Food and beverages will be on sale throughout in strict accordance with RSA guidelines. All persons purchasing alcohol must be 18 years or over, and provide identification if required.
Entry is by pre purchased tickets. Go to TryBooking
https://www.trybooking.com/book/event?eid=458934
Funds raised in 2018
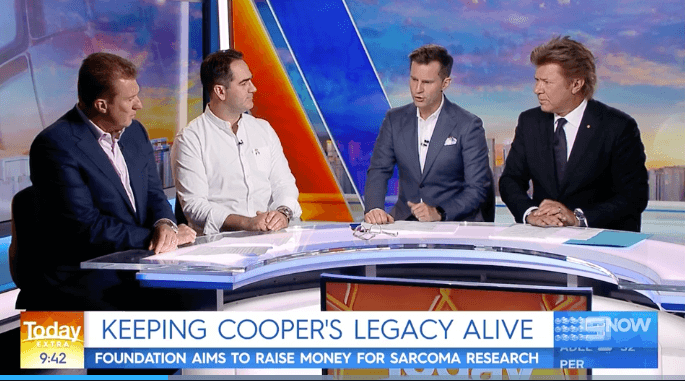
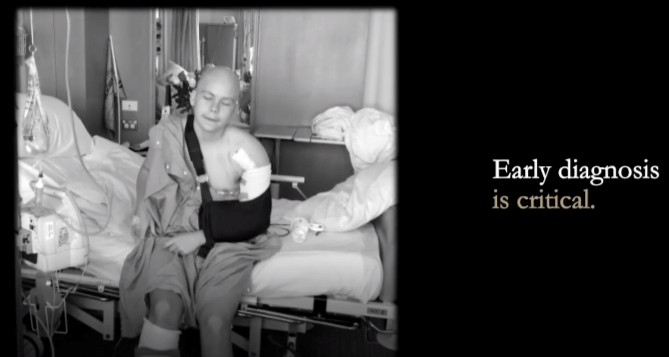
CRBF directors and our Medical Advisory Board unanimously voted to reinvest the funds raised by our hosted events, together with the extreme generosity of our major individual donors. At present we are in a consultative phase with research specialists, and leaders in the field of sarcoma, to establish where this significant amount of funding should be directed. As was Cooper’s vision, all funding will be directed to where it will have the most impetus – to positively change survival outcomes for sarcoma patients.
Farewell to our Chairman
When Jeremy Sutcliffe joined us as Chairman in 2018, we were aware his tenure would come to an end in 2019, due to his planned relocation to Europe for the year with his family.
Jeremy has provided a very strong start to our aims to positively change survival outcomes and treatment options for sarcoma patients. Through his wealth of expertise in the boardroom, as both an ASX 100 company chairman and as a seasoned company director. His strong passion for cause and personal experience with this cancer, has contributed to the
We wish to extend our heartfelt thanks to Jeremy for his belief in the work we are undertaking, and for the personal and professional qualities he brought to the role of Chairman.
We wish Jeremy and Catherine a safe, happy and healthy time overseas, making wonderful memories with their family.
Welcome to our new Chairman
CRBF would like to extend a very warm welcome to Justice Robert Beech-Jones, who will succeed Jeremy Sutcliffe, as our Chairman, effective immediately.
Robert brings a wealth of diverse experience to the role with proven leadership ability, experience at Board level and more significantly, in the not for profit sector, together with his very strong personal passion for cause, which is driven by his long association with Cooper through junior AFL.
To read more about Robert’s distinguished career, please visit our Board page at www.crbf.org.au.
Below an overview of CRBF’s first eleven months as a registered Australian charity, to provide you with a summary of what we have achieved to date, and our direction heading into 2019:
ACNC Registration
On Cooper’s birthday, January 22, 2018, our application for ACNC registration, and DGR status was approved, and the Cooper Rice-Brading Foundation became a registered Australian charity. This was bittersweet, as it was Cooper’s long-held aim to gain independence as a charitable entity, and was therefore tinged with immense sadness when he was unable to see it come into fruition.
Inaugural T20 Birthday Bash
Cooper’s long-time friend, and representative team mate, Will Todd, incepted the idea to host a cricket match on Cooper’s birthday, 2018, to pay homage to Cooper’s passion for cricket, and enabling the players, all from his days of school and representative cricket, commemorate the day while reliving memories from the past decade.
While the event was not designed as a fundraiser, sarcoma research benefitted from the $5000 it generated on the day, with special thanks to the Todd family, the players and volunteers who gave up their day, to Australian cricketer Nathan Lyon for his time and effort together with his manager, Peter Lovitt from the Drive Avenue Group, and to our partners, Costume Box, Coopers, Ties and Cuffs and Easts Cricket Club. The match was a huge success with the CRBF 1st X1 narrowly taking victory over the CRBF All Stars. 22 January, 2019 will see the second match played at Trumper Park.Oval, starting at 3 pm. A strictly limited number of tickets available at TryBooking – or by pressing the link below:
Mother’s Day Breakfast
Hosted by the dynamic Mia Freedman, this event was held on Friday 11 May, 2018, at Zest Waterside Venues, RMYC Point Piper. The breakfast was an outstanding success, raising in excess of $30,000 for clinical research for sarcoma. Due to its popularity, the event will be conducted once again in 2019. Our sincere thanks to major partners Glasshouse Fragrances, Dior, Zest Waterside Venues and Taylors Wines.
Robert Hao Piano Recital
Rob Hao very kindly dedicated his farewell performance to the Cooper Rice-Brading Foundation, prior to leaving to study an undergraduate Bachelor of Music, at the Royal College of Music in London. Rob kept the audience spellbound with works from Chopin, Bach and Alban Berg, finishing with an early Beethoven sonata. His immense talent and passion for music raised over $2000 to provide hope for young sarcoma patients, and we extend our heartfelt thanks to Rob for his kindness and generosity.
City To Surf
The Foundation’s first City to Surf proved to be highly successful both from an awareness and fundraising perspective. Thanks to the efforts of radio hosts Fitzy and Wippa together with NOVA 96.9, our campaign reached a national audience, and the CRBF team raised $20,000 as a result. The event also saw the release of our Stamp out Sarcoma merchandise, and caps, socks together with the “Run for Coops” t-shirts saw our team stand out for all the right reasons during the race. Our thanks go to Fitzy and Wippa, Nova FM, and Upcycle studio for their part in ensuring the campaign was an enormous success, together with the generosity of our sponsors.
Autore Pearls – “The Cooper”
Autore Pearls are synonymous with quality, and exquisite design, with their designs worn by Angelina Jolie, Halle Berry, Sarah Jessica Parker, and Selena Gomez, to name but a few.
The Cooper has been designed by AUTORE Design Director, Jane Autore, to embody the spirit, and the life of our precious son, whilst generating funding for critical clinical research by donating 10% of each sale directly to CRBF.
This is a unisex piece, with a magnificent Italian leather plaited band, an exquisite South Sea pearl, customised clasp with the CRBF logo, and a small garnet detail to signify Coops love of cricket. The bracelet is available in a double and single strand.
Our heartfelt gratitude to the Autore family, for creating this spectacular piece, and for their support of the work of CRBF.
SGS Trivia Evening
2017 saw the inaugural Sydney Grammar School trivia evening, with proceeds directed to CRBF. This was incepted by Senior Housemaster Mr Jason Slater, and supported by the form v1 boys. Sadly, Cooper was too unwell to attend, however was so very touched by the sentiment, as he would have been this year when the second trivia event was held, returning $1600 to clinical research into sarcoma.
Our sincere thanks to Mr Slater, together with Headmaster, Dr Richard Malpass, Masters and students for contributing to the success of this event.
Legends of League Chairman’s Dinner
The 11th September saw CRBF chairman, Jeremy Sutcliffe, host the Legends of League dinner, NRL Museum, NRL HQ. The league legends including Braith Anasta, Brad Fittler, Steve Blocker Roach, Wayne Pearce, Daly Cherry-Evans, Anthony Minichiello, Steve Edge and Michael Ennis dined with invited guests and share highly entertaining stories of their illustrious playing careers.
The evening was a resounding success returning $37,000 for clinical research into sarcoma, and our heartfelt thanks goes to the NRL commission, Todd Greenberg, Peter Beattie, Rachel Kramer and the NRL staff, together with host Anthony Maroon, and partners for the event, Serena Sanderson Catering and Dianna Jaber, director of Take Me, designer tableware.
The Griffith region NSW community fundraiser – Tayla Zandona
Tayla Zandona is a remarkable young woman who knows the heartache of sarcoma first hand, losing her big brother Kyle to this cancer on Christmas Day, 2016.
Despite the grief that never subsides, Tayla staged simultaneous events in the Griffith/Yenda region, to raise in excess of $4000 in an effort to ensure no other family ever go through the heartache she and her family live with daily. We will be working closely with Tayla this year in support of a very large event in this region. Having lost five members of the local community to sarcoma, this region is very committed to assisting the funding of sarcoma research, and we look very forward to working with this extremely generous group of individuals over the coming months.
We extend our heartfelt thanks to Tayla for her generosity of spirit. No-one can truly begin to understand the devastation of this cancer until you have witnessed a loved one fight so hard to conquer it – making her efforts truly inspiring.
Thank you
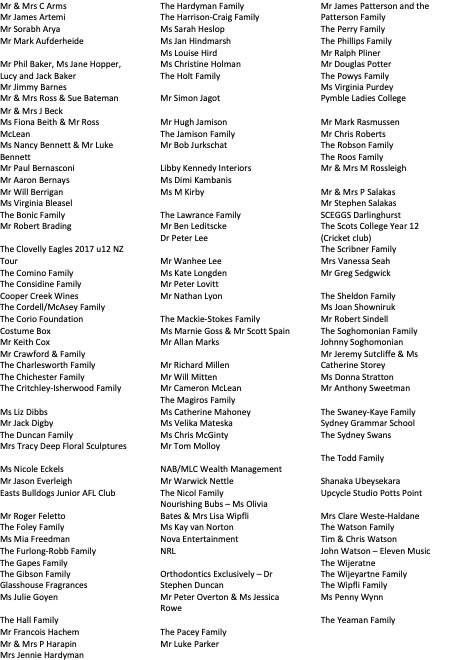
We would like to thank each of you, our donors, supporters, volunteers, directors and our executive committee members for the tireless work and support we have received throughout our first year as a registered charity.
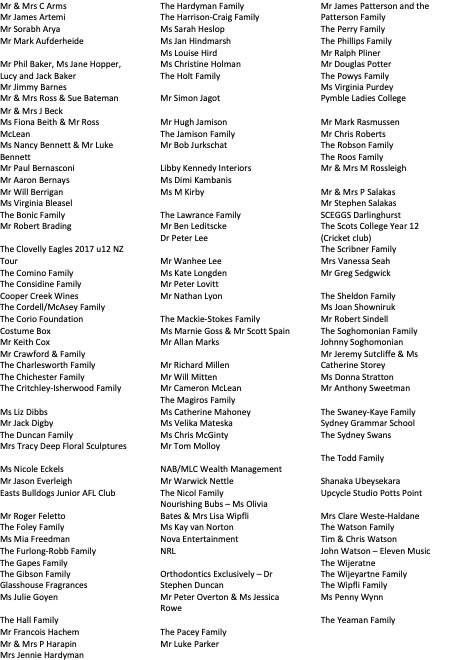
Special thanks to the following donors for their outstanding support.